5 Steps You Can Take to Speed Up Your Chronic Wound Healing
5 Steps You Can Take to Speed Up Your Chronic Wound Healing
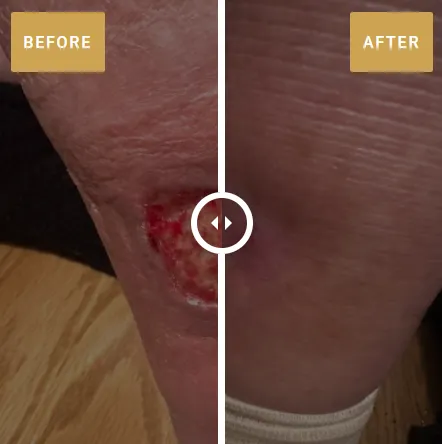
If you’re living with a chronic wound—like a diabetic foot ulcer, venous ulcer, or pressure sore—you know how tough it can be. The 10.5 million Medicare beneficiaries in the U.S. with chronic wounds face not just physical pain but also emotional challenges: fear of never healing, shame about your wound’s appearance, or feeling like a burden to your family. While medical care is essential, you have incredible power to support your body’s healing by making small, daily changes. By optimizing your internal environment through exercise, nutrition, mental health, sleep, and blood glucose control, you can give your wound the best chance to heal. Here are five evidence-based steps you can start today, whether you’re mobile or bedbound, to boost your recovery and reclaim your life.
Why Your Actions Matter
Chronic wounds affect 16.3% of Medicare patients and can lead to serious complications, like infections or amputations (82% of lower-limb amputations are linked to poor circulation, Diabetes Care, 2020). They also increase hospitalization risk by 20 times and cost $28.1–$96.8 billion annually (Journal of Wound Care, 2018). But studies show that lifestyle changes—like better nutrition or exercise—can improve healing rates by 15–25% (Wound Healing Society, 2022). Think of your body as a garden: medical care plants the seeds, but these steps enrich the soil to help healing grow.
Step 1: Move Your Body, Even a Little
Why It Helps: Exercise improves blood flow, delivering oxygen and nutrients to your wound, and reduces pressure on areas like your hips or heels. For diabetic patients (25% of veterans), it lowers blood sugar, aiding 30.5% of diabetes-related wounds (Diabetes Care, 2016). Even small movements prevent new ulcers, reducing progression by 40% (National Pressure Injury Advisory Panel, 2020).
What to Do:
If Mobile: Walk 5–10 minutes, 2–3 times daily (aim for 150 min/week, per CDC). Try chair exercises: 10 leg lifts or 20-second ankle circles, 2 sets.
If Bedbound: Do arm raises (10 reps) or leg extensions (5–10 reps/side). Reposition every 1–2 hours with caregiver help, using foam wedges ($15–$30).
Tools: Watch free “chair yoga for seniors” videos on YouTube or use a walker for safety.
Tips: Start with 1–2 minutes; track progress in a notebook. Consult your doctor first.
Why It Feels Good: Every move is a step toward independence, pushing back against the fear of being stuck forever.
Step 2: Fuel Your Body with Nutrition
Why It Helps: Protein rebuilds tissue, while vitamins and minerals fight infection and build new skin. Malnutrition delays healing in 30% of wounds (Advances in Wound Care, 2020). Hydration keeps skin supple, reducing breakdown risk.
What to Do:
Protein: Eat 1.2–2.0 g/kg body weight daily (90–150 g for 165 lbs): eggs (6 g/egg), chicken (26 g/3 oz), lentils (18 g/cup), or protein shakes (16 g/serving).
Vitamins/Minerals:
Vitamin C (500–1000 mg/day): 1 orange (70 mg) + 1/2 cup strawberries (60 mg).
Zinc (8–11 mg/day): 1 oz pumpkin seeds (2 mg) or 3 oz beef (7 mg).
Vitamin A (700–900 mcg/day): 1/2 cup sweet potato (1400 mcg).
Vitamin D (600–800 IU/day): 2 cups fortified milk (240 IU) or 10 min sunlight.
Hydration: Drink 8–10 cups water/day (64–80 oz); add lemon for flavor.
Tools: Use a grocery app (e.g., AnyList) for meal planning; buy affordable beans ($1/can) or eggs ($3/dozen).
Tips: Blend smoothies if chewing is hard; ask food banks for protein options. Work with a dietitian if possible.
Why It Feels Good: Nourishing your body is like giving it a healing hug, building strength from the inside out.
Step 3: Care for Your Mental Health
Why It Helps: Stress raises cortisol, slowing healing by 15–20% (Psychoneuroendocrinology, 2017). Depression affects 30–40% of wound patients, fueling isolation and shame (American Journal of Geriatric Psychiatry, 2020).
What to Do:
Practice 5–10 min/day of deep breathing (inhale 4 sec, hold 4, exhale 6) or guided meditation (Insight Timer app, free).
Join a support group (e.g., Wounds Canada online forum) or call a friend 1–2 times/week.
Journal 5 min/day about fears (e.g., “I’m scared of amputation”) in a notebook.
Ask your doctor for a counselor referral; Medicare covers up to 12 sessions/year.
Tools: Use free hotline (SAMHSA: 1-800-662-HELP) for support.
Tips: Start with 1 min of breathing; involve family in relaxation (e.g., calming music).
Why It Feels Good: Caring for your mind lifts shame and fear, helping you feel connected and hopeful.
Step 4: Prioritize Sleep
Why It Helps: Sleep boosts tissue repair and immunity, with poor sleep increasing infection risk by 15% (Sleep Medicine Reviews, 2018). Proper positioning reduces pressure ulcer progression by 30% (NPIAP, 2020).
What to Do:
Aim for 7–9 hours/night; nap 20–30 min if needed.
Create a sleep-friendly room: dark (blackout curtains, $10), quiet (earplugs, $5), cool (65–68°F).
Offload wounds: Use pillows for pressure sores (30° hip angle) or elevate legs for venous ulcers.
Avoid caffeine after 2 PM; limit screens 1 hour before bed.
Tools: Try a white noise app (White Noise Lite, free) or sleep tracker (Fitbit app).
Tips: Build a routine (e.g., 10 min reading); ask caregivers for positioning help.
Why It Feels Good: Sleep recharges your healing, giving you energy to face each day.
Step 5: Control Blood Sugar (for Diabetics)
Why It Helps: High glucose impairs healing, increasing infection risk for 30.5% of diabetic wounds. Stable levels (80–130 mg/dL pre-meal) improve closure by 20% (ADA, 2024).
What to Do:
Check blood sugar 1–2 times/day with a glucometer ($20–$50, Medicare-covered); target 80–130 mg/dL.
Eat low-glycemic foods: 1 cup quinoa (GI 53), 2 cups broccoli (GI 10); avoid soda (GI 63).
Take medications as prescribed; ask about Medicare Part D ($35/month insulin).
Inspect feet daily for new sores with a mirror or caregiver.
Tools: Log glucose with Glucose Buddy (free); join CDC’s free diabetes programs.
Tips: Plan meals with family; test A1C every 3 months (<7%).
Why It Feels Good: Controlling sugar puts you in charge, easing fears of complications.
Start Your Healing Journey Today
You have the power to support your healing with these five steps. Start small—maybe a protein snack or a minute of deep breathing—and build from there. For advanced wound care to complement your efforts, visit rebirthadvancedhealing.com to learn more and see if you qualify for specialized treatment. Your wound doesn’t define you—your strength does. Take one step today, and you’re on your way to recovery.
